Suicide prevention approach to be updated in light of COVID-19 and bushfire impacts
The Mental Health Commission of NSW will lead an update of the Strategic Framework for Suicide Prevention in NSW 2018-2023 in the wake of a series of destructive natural disasters and the COVID-19 pandemic during the past two years.
Australian Bureau of Statistics annual figures released today show that 876 people died due to suicide in NSW during 2020, at a rate of 10.5 suicides per 100,000 people. While this is a decrease from 937 suicide deaths at a rate of 11.4 per 100,000 in 2019, it is far too high and underscores the continued need for prevention to be a top priority.
NSW provides its own monthly reporting of suicides across the state through the Suicide Monitoring and Reporting System which provides estimates on suspected and confirmed numbers, using data collected from NSW Police and the State Coroner. This provides regular and timely information and records that in 2020 there were 896 people reported as suspected suicide deaths in NSW. This number varies slightly from the ABS report, which counts the number of people whose suicides have been confirmed or are being finalised through the coronial process. Taken together, they confirm that continued effort and focus is needed in the ongoing priority to reduce suicide in the community.
NSW Mental Health Commissioner Catherine Lourey said while it is too early to gauge the impact of the COVID pandemic or natural disasters based on the 2020 data released, there are a number of emerging trends creating concern.
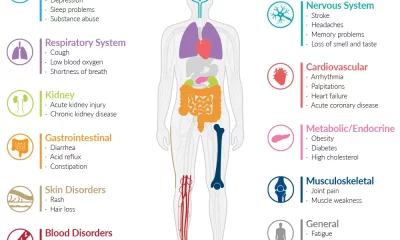
“While we do not yet have clear data on the impact of natural disasters and the COVID-19 pandemic on suicide rates, we are seeing increased demand for suicide prevention support services, increased mental health presentations in emergency departments, and greater use of mental health services booked through Medicare.
“Families, friends and communities across NSW are devastated by the impact of suicide, with an estimated 17 lives lost each week. These are not just statistics, each number is a person with their own story leaving bereaved loved ones behind. Tragically, suicide is the leading cause of death for people aged 15–44 years,” Ms Lourey said.
“In updating the Strategic Framework for Suicide Prevention in NSW the lived experience of people who have lived with suicidal thoughts or through a suicidal crisis, those bereaved by suicide and people caring for those who live with suicidal thoughts will be critical to our review. Together with other stakeholders and experts, we will be able to look behind the data to understand what’s really happening in our communities, what people’s own experience sheds light on and what types of interventions and support are most effective.”
The Strategic Framework for Suicide Prevention in NSW 2018-2023 launched in 2018 was followed by the Premier’s Priority Towards Zero Suicides Initiative which aims to reduce the suicide rate by 20 per cent from 2018 to 2023. This Initiative has provided $87 million to leading practice crisis care and support, building local community resilience and improving systems and practices to reduce the suicide rate in NSW. Additional funding has been provided in response to increased demand, including $8 million for programs in regional NSW.
The updated Framework will provide a set of key directions for a five year, whole of Government strategy to reduce the rate of suicide, draw upon best evidence and contemporary service approaches, build upon the work achieved under the Towards Zero Suicides initiative, and embed community responses and the voice of lived experience of suicide, suicidality, bereavement and caring.
Ms Lourey said consultation will begin shortly with people with lived experience, the community, the NSW Ministry of Health, lead Government agencies, the community managed sector and expert organisations.
Today’s ABS figures show suicide remains the leading cause of death among people aged 15-24, 25-34 and 35-44 years in NSW. The suicide rate of Aboriginal and Torres Strait Islander people at 21.6 is twice that of non-indigenous people which is 9.8. The suicide rate in rural and regional NSW is 15.4, which is twice that of Greater Sydney at 8.1. Involving these communities in the update of the Strategic Framework for Suicide Prevention will also be essential.
NOTE: The ABS counts suicides that have been confirmed or are being finalised through the coronial process while the NSW Suicide Monitoring and Data Management System provides estimates on suspected and confirmed suicides in NSW, using data collected from NSW Police and the State Coroner. See the latest NSW Suicide Monitoring System data at: https://www.health.nsw.gov.au/mentalhealth/resources/Publications/sums-report-jun-2021.pdf





 Tweed Shire News2 years ago
Tweed Shire News2 years ago
 Motoring News1 year ago
Motoring News1 year ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 Northern Rivers Local News3 years ago
Northern Rivers Local News3 years ago
 Health News3 years ago
Health News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 NSW Breaking News3 years ago
NSW Breaking News3 years ago