Prevention and early intervention critical to ending the cycle of family mental illness
An international group of researchers led by Monash University have developed a series of principles and recommendations to assist children whose parents are living with a mental illness.
The team of researchers have found that due to a range of factors, children whose parent/s have a mental illness are at risk for their own mental health problems and recommend that mental health services deliver support for the whole family and not only to individuals.
Children whose parents have mental illness are between two to 13 times more likely to develop a mental illness themselves, to be less school-ready, to present with higher rates of physical injury, more likely to be taken into care, and more likely to develop health conditions such as asthma.
Professor Andrea Reupert, from the School of Educational Psychology and Counselling in the Faculty of Education at Monash University, says children whose parents have mental illnesses are among the most vulnerable in our communities.
“Currently the delivery of evidence-based interventions to support these children have been limited by a lack of adequate support structures. We believe a major service reorientation is required to better meet the needs of these vulnerable children and their families. Accordingly, we’ve outlined a number of recommendations for practice, organisational and systems change to enable this,” said Professor Reupert.
The key recommendations outlined in the position paper, which was recently published in the Journal of Child Psychology and Psychiatry, include:
Child and adolescent-orientated services need to ask whether parents of clients have mental health concerns, ascertain the impact of the parent’s illness on the child, engage with parents to identify, and respond to, their needs and/or initiate and coordinate agency referrals for them
Adult orientated services should identify parenting status, engage with clients in their parenting role and responsibilities, engage with clients’ children to identify, and respond appropriately to their needs and/or initiate and coordinate agency referrals for children
Child and adolescent as well as adult-oriented services need to assess family strengths and needs, including the quality and quantity of family supports, parenting strengths and vulnerabilities, provide age-appropriate information about the parent’s mental illness to children, parents and other family members and consult with children and other family members when or if the parent is hospitalised, and monitor and follow up with of children and other family members, especially at key developmental milestones
Professor Darryl Maybery, from the Monash School of Rural Health in the Faculty of Medicine, Nursing and Health Sciences, says current practices need a complete overhaul so mental health support services are based on family needs rather than individualistic models of care.
“The paper specifically outlines the critical need for appropriate prevention and early intervention initiatives to be provided to children and parents living with parental mental illness. We provide clear direction to inform workforce and systemic change,” said Professor Maybery.
Professor Kim Foster, from the School of Nursing, Midwifery and Paramedicine at the Australian Catholic University, says the paper directly addresses recommendations from the National Mental Health Productivity Commission Report and the Royal Commission into Victoria’s Mental Health System, to provide child and adult mental health services that better meet the needs of these children and families.
“Applying the principles and recommendations from the paper will help services improve the quality of life and outcomes for children and families living with parental mental illness,” said Professor Foster.
Representing seven countries, the 24 authors of the position paper are research experts in the field of parental mental illness and are part of the Prato Collaborative for Change in Parent and Child Mental Health, which aims to contribute to the evidence base for these children and families and promote change at clinician, workforce, and systems levels.
To view the research paper, please visit: https://bit.ly/3ifJXNq





 Tweed Shire News2 years ago
Tweed Shire News2 years ago
 Motoring News1 year ago
Motoring News1 year ago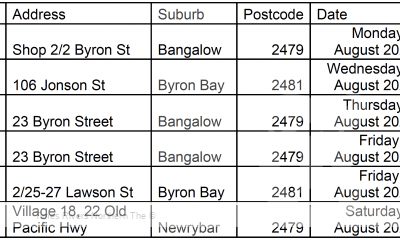
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 Northern Rivers Local News3 years ago
Northern Rivers Local News3 years ago
 Health News3 years ago
Health News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 NSW Breaking News3 years ago
NSW Breaking News3 years ago