Virtual reality is helping brain injury survivors regain use of their arms and hands
Survivors of brain injuries caused by stroke and other serious events can lose function in their arms and hands. An Australian company is creating a virtual reality therapy system to help survivors regain the use of these limbs.
Making brain injury therapy more engaging
Getting better after brain injury is hard work. Survivors need therapy to help the brain to heal. But therapy can be boring and repetitive. This means survivors don’t always do as much therapy as they need.
To make therapy more engaging, Australian company Neuromersiv has created the Ulysses VR Upper Limb Therapy System. Using a wireless virtual reality (VR) headset, brain injury survivors can do therapy by performing rewards-based, gamified activities in realistic environments.
An immersive environment
‘As soon as the person puts on the headset, they are totally immersed,’ CEO Anshul Dayal enthuses. ‘Like with gamers, dopamine kicks in and they want to keep going. So VR creates the motivation to keep doing your therapy. That can lead to better function recovery.’
The Ulysses VR software is available to buy in Australia and Britain. ‘I am proud we’ve taken this to market. We’re seeing people use it and give us positive feedback,’ Anshul says.
Wearable glove
As part of the Ulysses therapy system, Neuromersiv has also developed a hand and arm wearable glove. The glove helps users activate their muscles and receive real-time sensory feedback from VR environments. It combines two therapy modes with the VR software.
Functional electrical stimulation (FES) therapy helps brain injury survivors activate muscles they can’t move. Electrodes in the glove send small electrical currents through key points on the forearm muscles to stimulate extension and flexion.
New neural pathways
‘If the survivor is trying to brush their teeth in virtual reality but they just can’t grab the virtual toothbrush, the FES can assist with the grabbing action by stimulating flexion of the wrist and fingers,’ Anshul explains.
‘This stimulation creates a feedback loop that can be a catalyst for the brain to form new neural pathways to recover lost function. This is often referred to as brain neuroplasticity and is the key to long-term functional recovery.’

To make therapy more engaging, Australian company Neuromersiv has created the Ulysses VR Upper Limb Therapy System.
Sensory feedback
The team is also combining tactile feedback, or haptics, with the glove. For example, when users brush their teeth in virtual reality, they get a vibration effect on their fingers.
‘The goal is to enhance the sensory feedback because that helps the brain start to recognise the end of the fingertips, Anshul tells us. ‘When the person stops doing that task, they still feel tingling on the fingertips. That helps reactivate those neural connections.’
‘We are building a system that has multiple layers. Combining the visual and sensory aspects could improve functional recovery,’ Anshul concludes.
‘We think we are the first company in the world to combine FES, haptics and virtual reality.’
Technical challenges
The team had to overcome technical challenges to achieve this. Cameras on the virtual reality headset track users’ hands as they do therapy. The team’s first prototype had an exoskeleton design that impeded the hand tracking and overall usability. This was refined through user testing and design modifications.
‘For the FES, we created a sleeve with adjustable electrodes to wrap on the forearm,’ Anshul says. ‘For the haptics, we created a unique system of finger caps connected by soft & thin wires. It goes on top of the hand and doesn’t interfere with the tracking.
‘The next challenge was creating a wireless control unit for the glove that was compact and lightweight.’
Approval to sell the glove in Australia
Neuromersiv is planning a pivotal clinical trial to develop further clinical evidence on the safety and efficacy of the glove. With this evidence they will seek regulatory approval from the Therapeutic Goods Administration to commercialise the glove in Australia.
‘When you work with people in their homes and clinics, it can be confronting see the challenges they can face after the brain injury. That inspires me to help people through this Ulysses solution,’ Anshul says.
‘I have seen proof that when they use the system, they feel motivated and excited. They feel this can really help their therapy, and that’s quite rewarding.’
The MRFF-funded MTPConnect Biomedtech Horizons program funded Ulysses with $994,000.
For more seniors news, click here.





 Tweed Shire News2 years ago
Tweed Shire News2 years ago
 Motoring News2 years ago
Motoring News2 years ago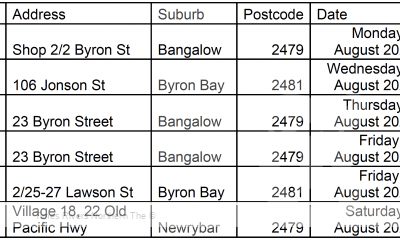
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 Northern Rivers Local News3 years ago
Northern Rivers Local News3 years ago
 Health News3 years ago
Health News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 NSW Breaking News3 years ago
NSW Breaking News3 years ago