Introduction of New Clinical Care Standard by ACSQHC to Address Psychotropic Medicine Use in Cognitive Disability and Impairment
By Jeff Gibbs
The Australian Commission on Safety and Quality in Health Care (the Commission) has today announced the launch of a pivotal new national standard aimed at enhancing the care for individuals with cognitive disabilities or impairments. The introduction of the Psychotropic Medicines in Cognitive Disability or Impairment Clinical Care Standard is a critical advancement in promoting safer and more effective treatment protocols across the healthcare spectrum.
Background and Rationale for the New Standard
Recent decades have witnessed a 60% surge in the prescription of psychotropic medications across Australia. Despite a modest reduction in antipsychotic use among the elderly—prompted by heightened awareness of associated risks—the prescribing rates remain alarmingly high, particularly among vulnerable populations. Notably, older individuals and those residing in aged care facilities are disproportionately affected by the adverse effects of these medications, including cognitive decline, heightened risk of falls, strokes, and mortality. Additionally, approximately one-third of individuals with intellectual disabilities are prescribed psychotropic drugs, exposing them to potentially severe short and long-term side effects.
Scope and Impact of the Standard
The new Standard seeks to mitigate the inappropriate utilisation of psychotropic medications and emphasises patient safety. It priorities non-pharmacological interventions as the foremost approach for managing challenging behaviours such as aggression and agitation. Psychotropic medications are advised as a last-resort measure, following the ineffectiveness of alternative strategies or in situations posing significant risk to the individual or others.
The Standard advocates for tailored non-medication strategies that respect the individual’s needs and preferences, developed in consultation with their family and other authorised caregivers. This approach underscores the commitment to upholding the dignity and autonomy of individuals with cognitive impairments.
Expert Insights and Support
Key health experts have endorsed the significance of this new Standard. Conjoint Associate Professor Carolyn Hullick, Chief Medical Officer at the Commission, stresses the necessity for mindful prescribing practices given the limited benefits and substantial risks associated with psychotropic medications in this demographic. Professor Julian Trollor from the University of New South Wales and Juanita Breen from the University of Tasmania also highlight the importance of objective-driven prescribing, continuous monitoring, and the potential to reduce medication dosages in favour of non-pharmacological alternatives.
Implementation Across Settings
The Standard is applicable universally across various healthcare settings, including hospitals, aged care facilities, and community services, ensuring that individuals with cognitive disabilities receive consistent and coordinated care irrespective of the setting.
Professor Eddy Strivens emphasises the need for coordinated efforts and effective communication, particularly during care transitions, to maintain continuity and efficacy of treatment plans and to support decision-making processes that honour patient autonomy.
Collaborative Efforts for Enhanced Care
In a collective endeavour to address these issues, the Commission has collaborated with the Aged Care Quality and Safety Commission and the NDIS Quality and Safeguards Commission to issue a Joint Statement against the misuse of psychotropics in managing behaviours in disabled and elderly populations.
Conclusion
The introduction of the Psychotropic Medicines in Cognitive Disability or Impairment Clinical Care Standard marks a significant step forward in improving the quality of care and safety for Australians with cognitive disabilities or impairments. It aligns with ongoing efforts to reform health care, aged care, and disability support systems across the nation.
The complete Standard and accompanying resources are available on the Commission’s website here.
For more seniors news, click here.





 Tweed Shire News2 years ago
Tweed Shire News2 years ago
 Motoring News1 year ago
Motoring News1 year ago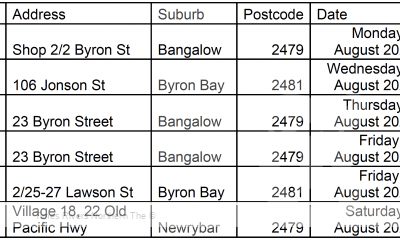
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 Northern Rivers Local News3 years ago
Northern Rivers Local News3 years ago
 Health News3 years ago
Health News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 NSW Breaking News3 years ago
NSW Breaking News3 years ago