UOW to train more future doctors for rural and regional Australia
GOVERNMENT, UOW COMMITMENT WILL SEE AT LEAST 30 STUDENTS START RURAL MEDICAL PROGRAM EACH YEAR
An extra 30 medical students will do their medical studies each year in the University of Wollongong’s end-to-end rural medical program as part of a $90 million Australian Government investment to support rural medical students nationally.
Students in the rural end-to-end program, undertake all of their studies in a rural or regional setting.
The Government is providing an additional 15 Commonwealth Supported Places to UOW each year for students to undertake the end-to-end rural medical program. The University will match and potentially exceed that number from its existing allocation of medical student places.
The additional places and funding were announced by Health Minister the Honourable Mark Butler MP today (4 December). The initiative is designed to train more students in rural areas in order to attract more doctors to work in regional and rural Australia.
Evidence shows that medical students who are placed for a year or more in rural and regional settings are more likely to stay and practise in rural and regional areas after they graduate.
The Government is also providing $16.3 million funding to UOW to invest in infrastructure and staff rurally, which will be used to increase medical classrooms, equipment, facilities and staffing to accommodate students in the end-to-end rural medical program.
Vice-Chancellor and President Professor Patricia M. Davidson welcomed the announcement, which recognised UOW’s successful track record in creating rural and regional medical specialists.
“The University of Wollongong is committed to improving the health and wellbeing of Australians living in rural settings,” Professor Davidson said.
“The UOW Graduate School of Medicine was set up to train doctors for rural, regional and remote areas, and was the first medical school in the country in which up to 70 per cent of students spend a full year of clinical education in a rural community.
“This announcement will enable us to expand our efforts to improve the quality of care given to patients in country hospitals and rural practices.”

An extra 30 medical students will do their medical studies each year in the University of Wollongong’s end-to-end rural medical program.
UOW Dean of Medicine Professor Zsuzsoka Kecskes said the Graduate School of Medicine was a recognised leader in the provision of medical education in rural areas.
“UOW is committed to a strong rural focus in our medical education program. Each year we know that a significant proportion of our alumni will choose to live and work in rural communities, which we are very proud of,” Professor Kecskes said.
“This investment by government allows UOW to strengthen and grow its high-quality education of medical students in rural communities, continue to invest in rural communities to ensure high-quality medical training for our students, which is a strong pathway to addressing the medical workforce shortages in rural areas.
“UOW commends the government on initiatives like this where universities can work with rural communities to embed medical education and ensure that future doctors continue to learn about, with and from communities.”
Senior Professor Eileen McLaughlin, Interim Deputy Vice-Chancellor (Academic and Student Life), said the government investment was testament to UOW’s regional and rural focus.
“The UOW medical program already has a strong rural focus with at least 56 per cent of its students having a rural background, and 70 per cent of students completing a year-long rural clinical placement, in communities including Milton/Ulladulla, Forbes, Mudgee, Grafton, Lismore, Griffith, Broken Hill, and elsewhere,” Professor McLaughlin said.
“Seventy-two per cent of all UOW medicine graduates who have attained specialty registration have specialised as General Practitioners and 40 per cent of these work rurally.”
There are UOW Graduate School of Medicine alumni practising in every Australian state and territory, from Kalgoorlie to Alice Springs to Cooktown, from Warrnambool to Yackandandah to Launceston, from Broken Hill to Grafton to Wagga Wagga.
For more rural news, click here.





 Tweed Shire News2 years ago
Tweed Shire News2 years ago
 Motoring News1 year ago
Motoring News1 year ago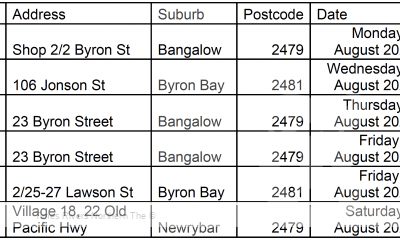
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 Northern Rivers Local News3 years ago
Northern Rivers Local News3 years ago
 Health News3 years ago
Health News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 NSW Breaking News3 years ago
NSW Breaking News3 years ago