Voice-assisted tech giving voice to people living with Parkinson’s disease
Monash University research has found voice-assisted technologies are able to support people with speech difficulties, such as Parkinson’s disease, and could enhance early speech and language therapies.
In 2018, over 1.35 million Australian households owned a smart speaker like Google Home and Amazon Alexa. While these technologies are primarily being used for general household tasks like streaming music, checking the weather forecast and setting alarms or reminders, new research has identified how these voice-assisted technologies can have additional uses for people with speech impairment.
A collaboration project by researchers at Monash University and Ulster University, this study is the first of its kind to explore the experiences of using voice-assisted technologies by people with speech impairment.
Of the 290 participants from the UK living with Parkinson’s disease who took part in the online survey, the key findings were:
-
- 90% owned a voice-assisted device
- 71% used it regularly
- 31% used the technology specifically to address the needs associated with their Parkinson’s disease
- Of these users, 55% sometimes, rarely, or never had to repeat themselves when using the technology and when asked about speech changes since they started using it, 25% of participants noticed having to repeat themselves less and 15% perceived their speech to be clearer
There are over six million people diagnosed with Parkinson’s disease worldwide and it’s currently the fastest growing neurological disease. Difficulties with speech occur in 90% of people with Parkinson’s disease, warranting a need for alternative methods of communication support.
Senior Lecturer in the Department of Human Centred Computing in the Faculty of Information Technology at Monash University, Dr Roisin McNaney, says the study demonstrates how these devices can help support future speech and language therapy outcomes.
“Early speech and language therapy intervention is important in addressing communication
issues related to Parkinson’s disease, however, only 59% of people living with Parkinson’s disease in Australia have regular contact with a therapist,” she said.
“The limited access to clinical services and speech therapies is a major concern and one that we hope to address through this research.
“By presenting our initial findings of how voice-assisted technologies can support speech and language therapy outcomes for people with Parkinson’s disease, we hope that we can encourage the future use of voice-assisted technologies by speech and language therapists in clinical settings to support patients.”
Low volume and reduced clarity are major symptoms of voice impairment in Parkinson’s disease and are routinely targeted in speech therapy. We had comments from participants during this study which directly indicated positive speaking behaviours from using the technology, such as “speaking slowly and clearly” and “talking louder” in order to ensure they are understood by the device. When asked what they would do if Alexa did not understand them, one participant simply said, “I’ll try again, a bit louder, until she understands me’.”
Dr Orla Duffy, Lecturer in Speech and Language Therapy at Ulster University, says voice-assisted technologies can offer long term benefits to people living with Parkinson’s disease.
“Voice-assisted technology has been embraced by many people and households, from both a general day-to-day perspective but also now, as we have seen from the research, in the form of assisting people with speech difficulties. Voice-assisted technologies now have the capability to support future therapies and act as useful tools for speech and language therapists, with the added benefit of already being present in the patient’s home,” said Dr Duffy.
While further research is needed to trial out-of-the-box voice-assisted technologies for speech and communication difficulties in people with Parkinson’s disease, the researchers hope that this study and its findings are a step in the right direction.
To find out more information about this project, please visit: https://rehab.jmir.org/2021/1/e23006





 Tweed Shire News2 years ago
Tweed Shire News2 years ago
 Motoring News1 year ago
Motoring News1 year ago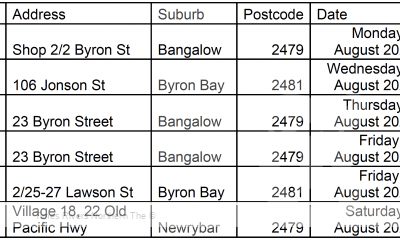
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 Northern Rivers Local News3 years ago
Northern Rivers Local News3 years ago
 Health News3 years ago
Health News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 NSW Breaking News3 years ago
NSW Breaking News3 years ago