Northern NSW emergency departments rated highly for care and cleanliness
Patients have rated Northern NSW Emergency Departments (EDs) among the best in NSW, according to the latest Bureau of Health Information (BHI) report which surveyed 77 of the bigger public hospitals across the state.
Results from the 2019-20 Emergency Department Patient Survey released today show that patients attending Northern NSW Local Health District (NNSWLHD) EDs continue to report high levels of satisfaction with their experience, health staff and facilities.
Most patients, 78 per cent, in the District reported being triaged within 15 minutes of arriving, the highest in the state.
The overall ratings of care by patients in the District were among the highest in the state, with 91 per cent of surveyed patients rating their care as ‘very good’ or ‘good’.
Patients rated ED staff highly with 93 per cent of patients rating the treatment provided by the ED health professionals as ‘good’ or ‘very good’.
NNSWLHD Emergency Departments also recorded high scores when it came to cleanliness, with 82 per cent of respondents saying the treatment area was ‘very clean’, the highest result in NSW for the second consecutive year. Byron Central Hospital recorded the highest rating of all NSW public hospitals for cleanliness with a 95 per cent result.
NNSWLHD Director of Clinical Operations, Lynne Weir, said the survey period included the emergence of COVID-19 in NSW in early 2020 which resulted in significant changes to the way health services were delivered.
“I want to commend our staff who continued to deliver outstanding results for our patients during a very challenging time for health services around the world,” Ms Weir said.
“It takes a dedicated team to deliver the quality experiences and outcomes our patients and the community expect, and these results are indicative of our commitment to patient care and to continuous improvement.
“For the second consecutive year, we achieved some of the best triage responses in the state and, importantly, we also rate among the top health districts for patient care measures.
“For example, our hospitals recorded excellent results when it came to asking patients if they felt they were able to get assistance or advice from ED staff for their personal needs, and 84 per cent said health staff ‘always’ explained things in a way patients could understand.”
A number of hospitals delivered improved results when compared with the previous year, with Ballina District Hospital in particular achieving significant improvements in 26 survey measures, including 99 per cent of surveyed patients reporting that they had confidence and trust in the ED health professionals treating them.
“These surveys are essential sources of information to help us identify gaps and develop plans to improve patient experiences at our hospitals,” Ms Weir said.
Between mid-2012 and mid-2020 the Northern NSW Local Health District increased its workforce by an additional 1008 full time equivalent staff – an increase of 26.7 per cent – including 171 more doctors, 367 more nurses and midwives, and 121 more allied health staff.
The 2020-21 budget for Northern NSW Local Health District was more than $926 million – an increase of almost $39 million, or 4.4 per cent, on the 2019-20 budget.
The record 2020-21 NSW Health statewide budget of $29.3 billion includes $30 million for additional emergency department attendances and ambulance calls and $14.5 million to recruit more temporary security staff and more patient experience officers to improve patients’ experiences in our public hospitals.
INDIVIDUAL HOSPITAL RESULTS
BALLINA DISTRICT HOSPITAL: The majority, 93 per cent, of surveyed patients rated their overall care as ‘good’ or ‘very good’. Nearly all patients, 99 per cent, said they had confidence and trust in the ED health professionals treating them, the highest in the state. The vast majority of those surveyed, 94 per cent, said ED health professionals were always kind and caring and 84 per cent said they were ‘definitely’ involved as much as they wanted to be in decisions about their care and treatment.
BYRON CENTRAL HOSPITAL: Nearly all surveyed patients, 95 per cent, said the ED was ‘very clean’, the highest rating in the state. More than 85 per cent of patients said they were triaged within 15 minutes and the majority, 80 per cent, said they would speak highly of their experience in ED to friends and family. In addition, 92 per cent rated their overall care in ED as ‘good’ or ‘very good’ and 85 per cent said the staff were always kind and caring.
CASINO & DISTRICT MEMORIAL HOSPITAL: The vast majority, 94 per cent, of surveyed patients said ED staff were ‘always’ polite and courteous and 87 per cent of patients said they were triaged with 15 minutes. More than 90 per cent of surveyed patients said ED health professionals ‘always’ explained things in a way they could understand and 98 per cent said their overall care was ‘good’ or ‘very good’.
GRAFTON BASE HOSPITAL: More than 85 per cent of surveyed patients said staff were ‘always’ kind and caring and the majority, 76 per cent, would ‘speak highly’ of their ED experience to family and friends.
LISMORE BASE HOSPITAL: Overall, 87 per cent rated the care they received as ‘good’ or ‘very good’. Nearly all patients, 97 per cent, said they felt the purpose of medication was explained in a way they could understand by ED staff and the majority, 78 per cent, reported that staff were kind and caring.
MACLEAN DISTRICT HOSPITAL: The majority of surveyed patients, 91 per cent, rated their care in ED as ‘good’ or ‘very good’. The vast majority, 92 per cent, said they felt treated with respect and dignity while in ED.
MURWILLUMBAH DISTRICT HOSPITAL: The vast majority of patients, 93 per cent, said ED staff explained things in a way they could understand and 88 per cent said they were triaged within 15 minutes. The majority, 84 per cent, said they had confidence and trust in the ED health professionals treating them and 95 per cent rated their overall care in ED as ‘good’ or ‘very good’. In addition, 93 per cent of respondents said the ED treatment area was ‘very clean’.
THE TWEED HOSPITAL: Overall, 90 per cent rated their care as ‘good’ or ‘very good’. The majority, 85 per cent, said they felt treated with respect and dignity and 78 per cent said they were triaged within 15 minutes.
The survey is available on the BHI website.





 Tweed Shire News2 years ago
Tweed Shire News2 years ago
 Motoring News1 year ago
Motoring News1 year ago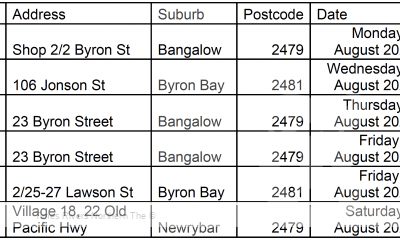
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 Northern Rivers Local News3 years ago
Northern Rivers Local News3 years ago
 Health News3 years ago
Health News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 NSW Breaking News3 years ago
NSW Breaking News3 years ago