‘Where was I going to find this money?’ – Cancer’s unseen side effect
UNSW Sydney
Finances need to be a bigger part of our conversation about cancer, UNSW Sydney researchers say.
When Jessie Oldfield was experiencing some bleeding at 23 weeks pregnant, she was worried that she had pre-eclampsia. But when the 28-year-old from Tumbarumba, NSW, turned up at the emergency department, the reality was so much worse.
“The doctor checked me all out and looked like she had run over my dog. Then she told me that I had cervical cancer,” Jessie says.
“When I heard that news, I was thinking, pre-eclampsia doesn’t look so bad now.”

Jessie Oldfield prior to her cervical cancer diagnosis. Photo: Supplied.
The next months would be a fight for Jessie and her baby’s survival. Jessie underwent multiple rounds of radiotherapy and chemotherapy, taking only a short break to give birth before returning to treatment.
The costs of receiving treatment quickly racked up. Jessie would regularly make the 90-minute drive to Wagga Wagga and the five-hour drive to Sydney for treatment. She received some support from Can Assist and the Isolated Patient Transport and Accommodation Assistance Scheme (IPTAAS), but paid the remaining travel and accommodation expenses out of pocket.
“I freaked out when I saw the costs. Where was I going to find this money? I’d just gotten pregnant,” Jessie says.
The treatments themselves were also expensive, with chemotherapy and radiotherapy only available through the private system in Wagga Wagga.
Thankfully, now both Jessie and her son Jack are doing well. However, Jessie worries about what will happen if her cancer returned.
“I’ve decided that if my cancer was to return or a new cancer found then I wouldn’t go through treatment because of how expensive it has been,” Jessie says.
“We simply can’t afford it, especially with the price of everything going up and now having a little one to look after.”

Jessie Oldfield with her partner Daniel after the birth of her son Jack. Photo: Supplied.
Financial toxicity of cancer
Jessie is one of many Australians who experience significant financial difficulties, or ‘financial toxicity’, due to cancer.
According to Dr Jordana McLoone from UNSW Medicine & Health and the Kids Cancer Centre at Sydney Children’s Hospital, financial toxicity goes beyond treatment costs.
“Financial toxicity is the negative patient impact coming from the cost of having cancer treatment. There are the direct costs of treatment as well as the indirect out of pocket costs related to your care and follow up, and potentially loss of income if time off work is needed,” Dr McLoone says.
People living outside of metro areas, as well as those who are already financially more vulnerable, are more likely to be affected by financial toxicity. However, as the cost of living goes up in Australia, this is likely to be an issue for more and more cancer patients.
Gaps in healthcare system
According to Dr McLoone, financial toxicity is a ‘blind spot’ within the cancer care system.
Dr McLoone has been conducting research as part of the Clinical Oncology Society of Australia (COSA) Financial Toxicity Working Group, to understand how healthcare professionals perceive and approach financial toxicity.
This is part of the working group’s broader program of research to define financial toxicity, scope current support services and resources, and develop solutions and innovations to address the issue. A key component of the working group’s research has been speaking with cancer patients (including Jessie) to understand what they are experiencing, and how they could be better supported.
Recently, Dr McLoone led a nationwide survey with Professor Louisa Gordon from QIMR Berghofer. They collected data from 277 Australian healthcare professionals in the field of oncology , including social workers, nurses, and medical specialists.
The survey analyses, published in Asia Pacific Journal of Clinical Oncology and Supportive Care in Cancer, show that 88 per cent of participants believed that discussions about financial toxicity are an important part of high-quality care.
“Healthcare professionals believed it was their responsibility within oncology care to have these discussions with families and to try and be as supportive as possible,” Dr McLoone says.
However, 28 per cent of health professionals said that they struggled to have financial toxicity discussions, because they lacked time during consultations and information about the topic. Also, some of the health professionals felt that there weren’t sufficient support services and resources to refer patients to.
“They feel they have no solutions to help patients that are sitting in front of them, very sick and very financially stressed,” Dr McLoone says.

Many Australians are unprepared for the financial toxicity of cancer. Photo: iStock.
Not a simple fix
According to Dr McLoone, training for healthcare professionals could be useful to enable them to talk to patients better about financial toxicity.
“This could involve education about the support services and resources available – but also the importance of just listening, acknowledging, validating and walking alongside the patient and their family,” Dr McLoone says.
However, to help patients with financial toxicity, there are also complex systemic issues that need to be addressed.
“There are certain issues that we weren’t even aware of until we started talking to patients. For example, you cannot apply for the Disability Support Pension unless you have a chronic, stable illness. And if you’re receiving cancer treatment, technically your illness hasn’t stabilised, so you’re ineligible,” Dr McLoone says.
Government, healthcare providers, patients and researchers will need to work together to identify and solve these gaps in support. Dr McLoone says that it is critical to address financial toxicity as for some patients, it can lead to truly poor outcomes.
“Some families have great support networks and they make it through and recover. But for some families, they do make difficult decisions like treatment abandonment. It’s a question of: do I feed my kids, or do I get my chemo?”
In May this year, the COSA Financial Toxicity Working Group, led by Professor Raymond Chan, hosted a National Think Tank on the topic of financial toxicity, bringing together researchers, health professionals, policy makers and patients. From these discussions the working group is developing a road map of the next steps to combat financial toxicity. Dr McLoone and others in the working group are optimistic about developing and implementing real solutions for patients and their families.
Cancer Council Helpline: 13 11 20 Cancer Council support resources

Dr Jordana McLoone, from UNSW Medicine & Health and the Kids Cancer Centre at Sydney Children’s Hospital, is researching the financial toxicity of cancer. Photo: Supplied.
Key facts:
– Many Australians experience significant financial difficulties, or ‘financial toxicity’, due to cancer – particularly now in the cost of living crisis
– E.g. our case study Jessie Oldfield, a 28 y.o. based in Tumbarumba, was diagnosed with cervical cancer at 23 weeks pregnant – had to cope with costs of treatment + travel to treatment + new baby
– Dr Jordana McLoone from UNSW researches financial toxicity. Her new research shows that 88% of health professionals believe they need to talk to patients about financial toxicity, but 28% lack the knowledge/time/resources for these conversations
– Managing financial toxicity is crucial to protect patients financially and prevent outcomes like treatment abandonment (which Jessie is sadly considering)
For more health news, click here.





 Tweed Shire News2 years ago
Tweed Shire News2 years ago
 Motoring News2 years ago
Motoring News2 years ago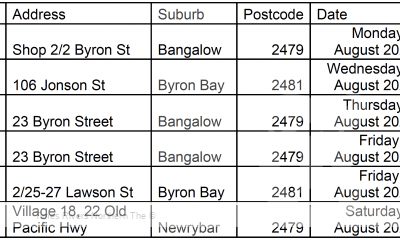
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 Northern Rivers Local News3 years ago
Northern Rivers Local News3 years ago
 Health News3 years ago
Health News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 NSW Breaking News3 years ago
NSW Breaking News3 years ago