Exploring the Relationship Between Psoriatic Arthritis and Raynaud’s Syndrome: Understanding Symptoms, Treatment, and When to Seek Medical Attention
Psoriatic arthritis (PsA) and Raynaud’s syndrome are distinct yet potentially overlapping conditions that can significantly impact an individual’s quality of life. While current research has not definitively established a direct link between them, individuals may experience both conditions simultaneously, necessitating a deeper exploration of their similarities, differences, and management strategies.
Understanding Psoriatic Arthritis (PsA)
Psoriatic arthritis is an immune-mediated inflammatory condition that affects approximately 30% of individuals with a history of psoriasis. It is characterised by joint pain, swelling, stiffness, and tenderness, often accompanied by symptoms such as eye inflammation, dactylitis (swelling of fingers or toes), and nail changes. Unlike rheumatoid arthritis, PsA pain tends to be asymmetrical, occurring on one side of the body. The frequency and duration of PsA flares vary among individuals, contributing to the complexity of its management.
Understanding Raynaud’s Syndrome
Raynaud’s syndrome, also known as Raynaud’s phenomenon, is a vascular disorder characterised by vasospasms in response to cold temperatures or stress. It primarily affects the fingers and toes, causing them to turn white, blue, or purple due to reduced blood flow. Symptoms may include numbness, tingling, or pain, which typically resolve when the affected areas warm up. Raynaud’s attacks can vary in duration, ranging from minutes to hours, and may be triggered by factors such as exposure to cold, emotional stress, or smoking.
Exploring the Relationship
While PsA and Raynaud’s syndrome can coexist in the same individual, current research has not identified a direct causal link between them. However, anecdotal reports and some studies suggest a potential association, particularly in the context of certain biologic therapies used to treat PsA. Further investigation is needed to elucidate any underlying connections between these conditions and their shared pathophysiological mechanisms.

Psoriatic Arthritis and Raynaud’s Syndrome indicators.
Treatment Strategies
The management of PsA and Raynaud’s syndrome aims to alleviate symptoms, reduce disease activity, and prevent long-term complications. Treatment options for PsA may include nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), biologics, physical therapy, and lifestyle modifications. Similarly, Raynaud’s syndrome treatment may involve medications that improve blood flow, such as calcium channel blockers or vasodilators, along with lifestyle adjustments to minimise triggers.
When to Seek Medical Attention
Early diagnosis and intervention are crucial for effectively managing both PsA and Raynaud’s syndrome. Individuals experiencing symptoms such as joint pain, swelling, stiffness, or changes in skin colour should promptly consult a healthcare professional, particularly a rheumatologist specializing in autoimmune conditions. Additionally, individuals with Raynaud’s syndrome should be vigilant for signs of complications, such as ulcers or cardiovascular issues, and seek medical attention if warranted.
Conclusion
While Psoriatic arthritis and Raynaud’s syndrome present unique challenges, understanding their symptoms, treatment options, and potential overlaps is essential for providing comprehensive care to affected individuals. By raising awareness and promoting further research into the relationship between these conditions, healthcare professionals can better support patients in managing their symptoms and improving their overall quality of life.
For more health news, click here.





 Tweed Shire News2 years ago
Tweed Shire News2 years ago
 Motoring News1 year ago
Motoring News1 year ago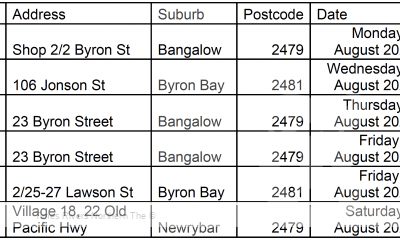
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 Northern Rivers Local News3 years ago
Northern Rivers Local News3 years ago
 Health News3 years ago
Health News3 years ago
 COVID-19 Northern Rivers News3 years ago
COVID-19 Northern Rivers News3 years ago
 NSW Breaking News3 years ago
NSW Breaking News3 years ago